What is PCOS? Causes and Treatment of Polycystic Ovary Syndrome
Key highlights:
- PCOS is a complex hormonal disorder that affects millions of women in their reproductive years, leading to irregular periods, excess androgen (a steroid hormone such as testosterone that controls masculine characteristics), and polycystic ovaries.
- The condition is linked to insulin resistance, low-grade inflammation, and genetics in PCOS, which can impact overall female reproductive health and long-term well-being.
- Women with PCOS may experience fertility problems, pregnancy complications, acne, thinning scalp hair, and excess facial hair. Increased risk of heart disease, sleep apnea, and endometrial cancer risk occurs if left untreated.
- While there is no permanent cure, a PCOS diagnosis can be treated and even reversed through diet and lifestyle changes, medications, and weight management, which enables women to lead healthy and balanced lives.
What is PCOS?
At its core, Polycystic ovary syndrome (PCOS) is a problem of hormones that leads to an imbalance in the body. Women with PCOS often experience irregular periods because their ovaries struggle with irregular ovulation. Instead of releasing mature eggs, the ovaries may hold on to immature eggs, which remain trapped inside small sacs. These sacs are known as follicles in the ovaries, and over time, they create cysts in the ovaries, a hallmark of the condition.
The symptoms extend beyond the ovaries. High levels of excess androgen (male hormones) often cause severe acne, excess facial and body hair (hirsutism), or even male-pattern baldness in women. Some women also notice dark, velvety skin patches (acanthosis nigricans), which point toward insulin resistance and PCOS. These visible signs make PCOS both a medical and emotional challenge.

What does PCOS mean, and why is it called Polycystic Ovarian Syndrome?
The name “Polycystic ovaries” can be misleading. Many assume it refers to multiple harmful cysts, but in reality, it describes the
polycystic ovarian changes where eggs remain trapped in fluid-filled sacs. These are not dangerous cysts but
immature eggs that fail to mature or be released. This inability to ovulate regularly explains why
infertility in women with PCOS is a common challenge.
Doctors use the term “syndrome” because PCOS involves more than one symptom. It includes hormone changes, metabolic issues like metabolic syndrome, and physical signs such as acne or weight gain. So, while the name focuses on the ovaries, the syndrome itself affects overall female reproductive health and beyond.
How does PCOS affect a woman’s health beyond just the ovaries?
The influence of PCOS goes well beyond the ovaries. For example, insulin resistance is one of the most consistent features of this condition. When your body struggles to use insulin properly, it increases blood sugar levels, which often leads to weight gain with PCOS. Over time, this problem is tied to obesity and PCOS complications, such as metabolic dysfunction-associated steatosis (MASLD), sleep apnea, and even heart disease risk in women with PCOS.
PCOS also has a strong emotional and mental impact. Studies show that women with the syndrome are at higher risk for depression and anxiety, mostly due to body image struggles, fertility concerns, and chronic health issues. These problems highlight that PCOS is not just about reproduction but about long-term wellness and mental stability.
Who Does PCOS Affect?
PCOS mainly affects women in their reproductive years, but the severity differs from one woman to another. In the USA, it is estimated that nearly 5 million women have PCOS, making it one of the most common endocrine disorders in this age group. Risk factors include obesity and PCOS complications, a family history of PCOS, and existing issues with insulin resistance.
Does PCOS affect women of all ages or only during reproductive years?
Although most cases appear after puberty, symptoms can continue well into later life. Even after menopause, women may carry higher heart disease risk in women with PCOS, face problems with metabolic syndrome, or experience long-term hormonal imbalances. This makes PCOS a lifelong condition requiring ongoing attention.
Can women without a family history of PCOS still develop the condition?
Yes, genetics do play a role PCOS, but they are not the key contributor. Women without a genetic predisposition can still develop PCOS due to low-grade inflammation, poor dietary habits, or hormonal triggers. This explains why some women face fertility problems in women even when their family has no history of the disorder.
When Does PCOS Usually Start?
The first signs of PCOS usually show up around puberty, when young girls begin menstruation. Symptoms like irregular periods, heavy bleeding, and severe acne may indicate a hormonal imbalance. Sometimes, these early signs are overlooked as “normal teenage changes,” leading to delayed PCOS diagnosis and treatment.
Can PCOS develop later in life, or does it usually begin around puberty?
While most women notice symptoms during their teenage years, PCOS can appear later, especially if triggered by weight gain, stress, or other health changes. Some women in their twenties or thirties may suddenly develop menstrual irregularities, making it clear that the condition can evolve over time.
As women age, symptoms may shift. While irregular ovulation and fertility problems in women dominate younger years, older women face higher risks of gestational diabetes, pregnancy complications, and later endometrial cancer risk. These shifts remind us that PCOS is not static—it changes with the body’s needs.
Where Does PCOS Affect the Body?
Is PCOS only about the ovaries, or does it impact other parts of the body too?
Although the name points to the ovaries, PCOS affects the entire body. Women with this condition often deal with low-grade inflammation, insulin resistance, and problems related to metabolic syndrome. These issues create risks for heart health, weight management, and even liver function.
How does PCOS influence skin, hair, and weight?
Visible signs include severe acne, male-pattern baldness in women, and excess facial and body hair (hirsutism). Many also struggle with weight gain with PCOS, which is harder to manage due to insulin resistance. For some, even strict diets and exercise routines provide limited results, increasing frustration and emotional stress.
What role does metabolism play in PCOS?
PCOS and metabolism are deeply connected. The inability to handle sugar properly leads to metabolic syndrome, which increases the risk of heart disease risk in women with PCOS. This explains why weight management in PCOS is so crucial—it’s not only about appearance but also about long-term health.
Why Does PCOS Happen?
What are the main causes behind PCOS?
The exact cause of PCOS remains unknown, but research shows that insulin resistance, high androgen levels, and low-grade inflammation are all major contributors. These factors create an environment where follicles in the ovaries cannot release eggs, leading to polycystic ovarian changes.
Is PCOS more genetic, hormonal, or lifestyle-related?
It is a combination of all three. Heredity and genetics in PCOS increase risk, but poor diet and stress can trigger symptoms in genetically vulnerable women. This is why two women with similar family histories may have completely different outcomes.
Why do some women develop PCOS while others don’t?
The difference lies in how hormones and the environment interact. Some women carry the genetic tendency but never face fertility problems in women, while others without a strong family background may still develop the disorder due to lifestyle or obesity and PCOS complications.
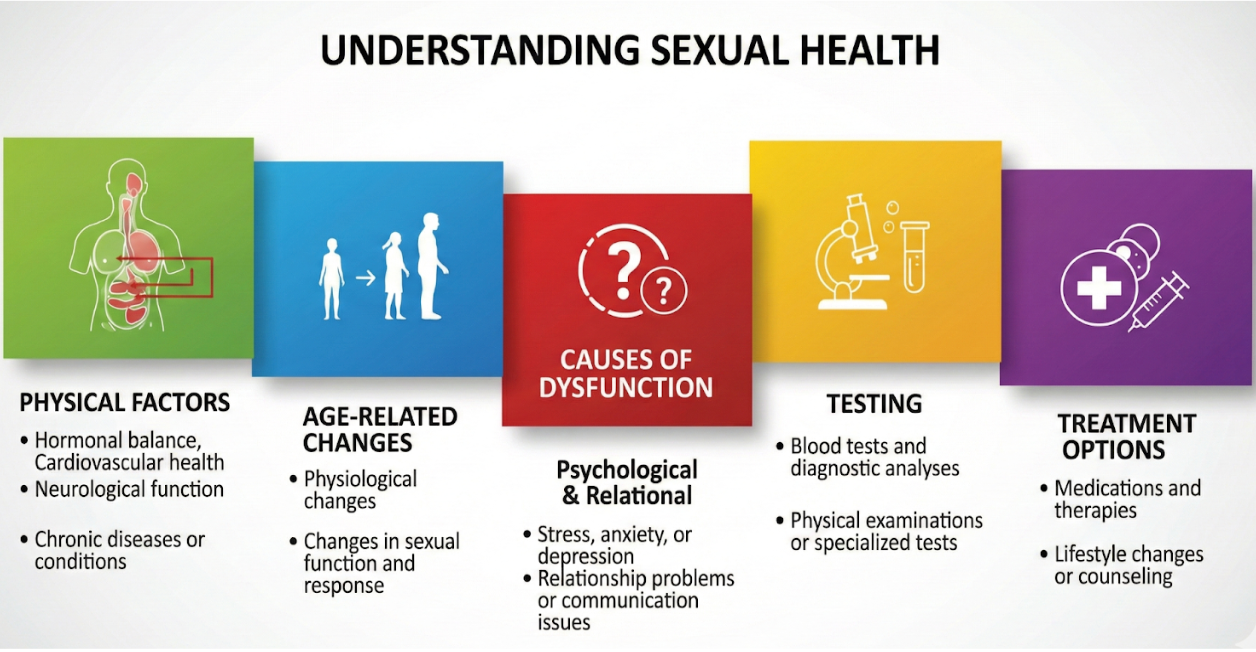
How is PCOS Diagnosed?
How do doctors check if someone has PCOS?
Doctors start with a detailed medical history and physical exam, focusing on signs like irregular periods, excess androgen, or cysts in ovaries. A patient’s weight, acne, and hair growth patterns are also important clues.
What tests are used to diagnose PCOS?
Common tools include blood tests to measure hormones like insulin, testosterone, sex hormone binding globulin, and metabolic biomarkers such as hemoglobin A1C, glucose, and cholesterol. Ultrasound scans check for polycystic ovaries and immature eggs trapped in the follicles. Together, these findings form the basis of a PCOS diagnosis and treatment plan.
How important is early diagnosis for managing PCOS?
Early detection is critical. Without it, women face long-term complications of PCOS, such as gestational diabetes, sleep apnea, and even endometrial cancer risk. Identifying the condition early allows better planning for weight management in PCOS, lifestyle improvements, and fertility care.
How is PCOS Treated?
Treatment depends on the symptoms. Birth control pills regulate irregular periods, while medications for insulin resistance reduce metabolic risks. Fertility drugs help women who face infertility in women with PCOS. Each treatment plan is customized based on the patient’s goals.
Can lifestyle changes help manage PCOS naturally?
Absolutely. Weight management in PCOS through healthy eating and exercise reduces insulin resistance, lowers excess androgen, and improves overall health. Stress management is equally important because stress worsens hormonal imbalance in women.
Diet and lifestyle changes can often reverse PCOS. By combining lifestyle changes with medical care, women can reduce long-term complications of PCOS and live healthy lives.
What Are the Outcomes of PCOS?
Can women with PCOS still get pregnant and have healthy children?
Yes, many women with PCOS can still get pregnant, although it may take more time and care. With the right medical support and lifestyle changes, women can overcome fertility challenges and go on to have healthy pregnancies. Treatments for conditions like gestational diabetes also help ensure safer outcomes for both mother and baby.
Untreated PCOS can lead to serious health concerns, including heart disease, fatty liver, depression, anxiety, and a higher risk of endometrial cancer. This is why early care and ongoing treatment are so important.
By focusing on a balanced diet, regular exercise, and emotional well-being, women can manage PCOS effectively. With proper treatment, awareness, and consistent follow-up, it is possible to live a healthy and fulfilling life despite the condition.

Conclusion:
PCOS is more than a reproductive issue; it is a condition that influences every part of a woman’s health. From irregular ovulation to long-term complications of PCOS, the journey may seem overwhelming, but knowledge is power. With the right PCOS diagnosis and treatment, lifestyle changes, and medical support, women can take control of their health, manage symptoms, and reduce risks.
FAQs:
1: What does PCOS do to a woman?
PCOS can cause hormonal imbalance, leading to irregular periods, weight gain, acne, excess hair growth, and sometimes fertility problems. It can also raise the risk of diabetes and heart disease if not managed.
2: What are the first signs of PCOS?
The first signs often include irregular periods, acne, weight changes, and extra facial or body hair. Some women may also notice hair thinning on the scalp or dark skin patches.
3: Can a PCOS girl get pregnant?
Yes, women with PCOS can get pregnant, but it may take longer due to irregular ovulation. With treatment, lifestyle changes, and sometimes fertility medicine, many women go on to have healthy pregnancies.
4: What is the main cause of PCOS?
The exact cause isn’t fully known. But
hormonal imbalance, genetics, insulin resistance, and lifestyle factors all play a role in developing PCOS.